56Y male Patient with COVID PNEUMONIA
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of the case
CASE:
Fever since 10 days
Cough since 9 days
Shortness of breath since 7 days
HOPI
Patient was apparently asymptomatic 11 days back, he is additional security inspector by occupation in his daily routine, he wakes up at 5 AM and starts at 6.30 AM to Hyderabad travel by bus around 120 kms to reach his work place by 9 AM changes multiple busses to reach destination, his routine work in the security office block mostly consist of written work and then he starts again back to home by 5 PM changes multiple busses and reaches home back by 8 PM and by routine he sleeps around 10 PM. Everything was normal 11 day's back then he first developed
FEVER on 26/04/2021 which is insidious in onset, continuous, High grade associated with chills and rigors, no diurnal variation, no aggrevating factors and
Relieved with medications
COUGH
Patient developed Dry cough which is insidious in onset, gradually progressive in nature, not associated with sputum, aggrevated by talking and on exertion and not relieved by medication.
SOB : Insidious in onset, gradually progressive in nature,(MMRC grade 0 to 2) aggrevated with cough and relieving on rest and O2 supplementation, no postural and diurnal variation
No history of wheeze
No h/o cold
No h/o haemoptysis
No h/o PND/orthopnea
No h/o loss of appetite
No h/o joint pains/ early morning stiffness of fingers
On 26/05/2021 he developed fever still he managed to go to daily routine work to office by taking paracetamol tablets
On 28/5/2021 he gave samples & he was tested positive for RTPCR & Rapid antigen test for COVID
So he was advised home quarantine and medications in other hospital, he used to take rest during the Home quarantine period in isolated room used to sleep for 8-10 hrs these days at home and high protein diet. Spending time with newspapers and Mobile.
He was given following medications on 28/05/2021,
1) TAB. FABIFLU 1800 mg BD on day 1 and from day 2-9 800 mg BD
2) Tab. Ivermectin 12 mg od
3) Tab. Doxy 100 mg BD
4) Tab. DOLO 650 mg TID
5) TAB. VIT C 500 MG OD
6) TAB. VIT D 60k IU Weekly once
7) Tab Zincovit od
8) Syrup. ASCORYL 15 ML TID
On 3/05/2021 He was admitted in a private hospital in Hyderabad as Symptoms were not relieving and treatment was given.
On 04/05/2021, He received 200 ml IV plasma therapy for two days and following treatment was given
1) Inj. Remdesivir 200mg iv stat on day 1 and 100 mg iv od for 4 days
2) Inj Cefipime TZ 1.125 g iv bd
3) Inj Doxycycline 100 mg iv bd
4) Inj. Methylprednisolone 125 mg iv bd
5) Inj.Clexane 40mg sc od
6) Inj. Optinueron 1 amp in 100 ml NS iv OD
7) Continous Oxygen supplimention 6-8 L
8) Nebulization with budecort and mucomyst was given 4 th hourly
On 07/05/2021
He was discharged as Lama in that hospital due to financial issues and poor satisfaction of the patient and was admitted in our hospital at 7 PM
PAST HISTORY
No h/o Diabetes, systemic hypertension, bronchial asthma, pulmonary koch’s, epilepsy, CVA, CAD, and Thyroid disorder
Personal History
Diet: Balanced
Appetite: Normal
Bowl/Bladder:Regular
Sleep: Disturbed
Addictions: Non smoker and non alcoholic
Family history
History of similar complaints in the family (wife and elder son ) and was diagnosed as COVID 19 viral pneumonia and treatment was given in home isolation.
Summary:
A 56 year old male Patient with Fever, cough and sob since 10 days, which is Acute respiratory illness, involving lung parenchyma, infectious in etiology.
GENERAL EXAMINATION
Patient conscious, coherent, cooperative, comfortably sitting in chair .
Moderately built and moderately nourished
Height-170cms Weight-70kgs
BMI-(24.2)
No pallor, No icterus,
no cyanosis, no clubbing ,
no lymphadenopathy, no edema,no koilonychia
VITAL DATA:
Temp: 100.2 F
PR: 132/min regular, normal volume, normal character, no radio radial and no radio femoral delay
BP: 110/70mmhg im right upperlimb in sitting position
RR: 28 breaths/min, regular abdomino thoracic type of breathing
Spo2 : 82 on RA and 95 on 8L of O2
Respiratory system Examination
Inspection:
Upper respiratory tract is normal
Chest is Bilaterally symmetrical in shape, no scoliosis , no kyphosis, No Inter costal fullness ,Trachea appeared to be central.
Apical impulse not visible.
Accessory muscles ( abdominal muscles) usage
is seen,
No chest indrawing, No widening of intercostal spaces or overcrowding of ribs
No visible pulsations and engorged viens , No visible scars, sinuses, and swellings
No drooping of shoulders.
Palpation:
All inspectory findings are confirmed.
Tracheal position central.
No local raised temperature
, No Tenderness noted, apex beat is felt in the precordium left 5th intercostal space, half-inch medial to the left midclavicular line, Respiratory movements equal on both sides.
Percussion:
Direct percussion : Normal
Indirect percussion :
Dullness is noted in Left infraclavicular left mammary and inframammary, and infraaxillary and infrascapular areas
And in the right side, dullness is noted in infraaxillary and infrascapular areas.
AUSCULTATION:
Bilateral air entry is present.
Bronchial breath sounds heard in inframammary, infraaxillary infrascapular areas of both sides.
And coarse crepitations heard in the above Areas.
Other systems examination
CVS: S1,S2 heard, no murmers
GIT: non tender, no organomegaly
CNS: no abnormality detected
Investigations:
Outside hospital investigations on 5/5/21
CBP :
Hb : 14.3 g/ do
TLC: 4300
Platelets: 1.63 L
Peripheral smear: Normocytic and normochromic.
Blood group : O + ve
RFT :
Sr creatinine : 0.9 mg/ dl
Sr. Urea 18 mg/ dl
IL - 6 : 6.3 pg/ml [ normal: 0 - 4.4]
D DIMER :. 462 ng/ml. Normal (<500)
CRP : 80.54 mg/L ( normal is <6)
LDH : 321 IU/L ( 208 - 375)
FERRITIN : 224ng/L
CRP repeat 27.9mg/L (0-6)
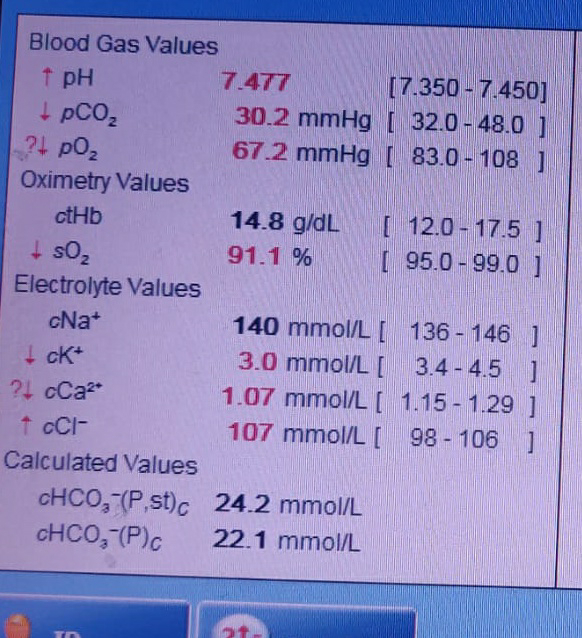
Our hospital investigations :
8/05/2021
Supine position AP VIEW CxR on 11/05/2021
PROVISIONAL DIAGNOSIS:
ACUTE INFECTIVE CONDITION OF LUNG PARENCHYMA, most probably due to SARS-COVID 19 VIRAL PNEUMONIA.
Treatment given in our hospital: on admission day:
1) Inj. Augmentin 1.2 g iv bd
2) Inj. Clexane 40 mg sc od
3) Inj. Dexamethasone 8 mg iv tid
4) O2 supplementation 6-8 L via nasal prongs and oxygen mask with reservoir bag.( Non rebreathing mask)
5) Nebulization with budecort and mucomyst 4 th hourly and 6th hourly respectively
6)Inj. Pantop 40 mg iv OD
After two days we had following changes:
1) Tab. Augmentin 625 mg po BD
2) Tab. PANTOPRAZOLE 40 MG OD
3) TAB. METHYLPREDNISOLONE 16 MG BD
4) O2 SUPPLEMENTATION via Non rebreathing mask
We discharged our patient on 12/05/2021
Thank you




























Comments
Post a Comment